SEPTIC
ABORTION:
Suspected septic abortion with RPOC is a medical emergency, and management should be immediate. The
uterus should be evacuated promptly after initiating antibiotics and
stabilizing the patient in cases of suspected septic abortion or RPOC as delay
may be fatal. Suction curettage is less traumatic than sharp curettage. If the
patient fails to respond to uterine evacuation and antibiotics, a pelvic
abscess or clostridial necrotizing myonecrosis, although rare, should be
suspected. In such case, laparotomy and possible hysterectomy might be
considered.

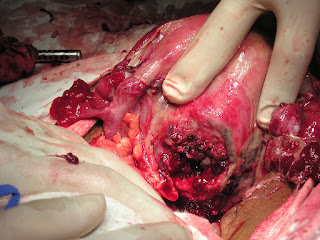
fig 1.1 SEPTIC ABORTION

fig 1.1 SEPTIC ABORTION
Abortion with septic shock
Abortion with septic shock is a medical emergency. An
abortion is a procedure that ends a pregnancy. Septic shock occurs when an
infection overtakes your body and causes very low blood pressure.
Septic shock can affect anyone susceptible to the germs
that cause infection. When linked with abortion, septic shock can be a
dangerous complication.
Types of abortions
There are several types of abortions:
A spontaneous abortion (miscarriage) occurs when
pregnancy tissue is passed from the body. There are technically two types of
spontaneous abortions: “complete,” in which all the pregnancy tissue is passed
and no intervention is needed, and “incomplete,” in which only part of the
pregnancy tissue is passed and it usually does require intervention.
A surgical abortion is the removal of the fetus and
placenta from the woman’s uterus. The doctor typically uses a vacuum to extract
the pregnancy material.
fig 1.2 SEPTIC ABORTION
A medical abortion uses prescribed medications. These
medications help the mother pass the fetus and related tissue. The result is
similar to a miscarriage.
A self-induced abortion is done by the mother herself.
This term includes both abortions conducted through legal, over-the-counter
medication and those performed through unregulated, often dangerous methods.
Advertisement
Symptoms of abortion with septic shock
Symptoms
Septic shock is a medical emergency. If you recently had
an abortion and experience any of the following symptoms, seek medical help
immediately:
fig 1.3 Symptoms of abortion with septic shock
- Very high or very low body temperature
- Heavy bleeding
- Severe pain
- Cool, pale arms and legs
- Feelings of confusion, restlessness, or fatigue
- Shaking chills
- Low blood pressure, especially when standing
- Inability to urinate
- Heart palpitations
- Rapid, pounding heart rate
- Difficult, rapid breathing with shortness of breath
Causes of abortion with septic shock
Causes
Septic shock often occurs after the abortion procedure is
completed. It strikes when your body becomes contaminated with a bacterial
infection.
In most cases, the infection stays in a specific area.
However, in more severe cases, the infection enters your bloodstream and
travels throughout your body. This is called a systemic reaction. The resulting
condition is called sepsis.
Your body’s initial reaction to sepsis typically involves
very low or very high body temperatures. In addition, sepsis causes:
- Rapid heart rate
- Rapid breathing rate
- Very high or very low white blood cell count
- As sepsis weakens your body’s immune responses, your organs begin to fail. When sepsis worsens so that your blood pressure drops dangerously low and is immune to treatment, the condition is called septic shock.
In abortions, two main factors can contribute to the
onset of sepsis and ultimately, septic shock. They are:
An incomplete abortion: pieces of the pregnancy tissue
remain in the body after a spontaneous or induced abortion, both medical and
surgical
bacterial infection in the uterus during a surgical or
self-induced abortion
Risk factors for abortion with septic shock
Risk Factors
Your risk for septic shock is increased in situations
where bacteria are more likely to enter your bloodstream. Having any surgery or
medical procedure puts you at an increased risk for septic shock.
When medical devices are inserted into your body, the
device can introduce bacteria. This makes infection and sepsis more likely. The
longer the device is in your body, the higher your risk for infection.
In a surgical abortion, the doctor uses a vacuum with a
hollow tube to remove the fetus and placenta from the womb. Medical devices,
such as catheters, drainage tubes, or breathing tubes can put you at a similar
risk of infection.


fig 1.6 Abortion of septic shock
The risk for septic shock is significantly increased in
self-induced abortion, where medical instruments are not used. There is less
ability to prevent germs from spreading because many of the common tools are
everyday household items and are not sterile.
In addition, having certain underlying conditions prior
to an abortion can make you more susceptible to septic shock. They include
having a chronic condition such as diabetes or a weakened immune system.
Most medical abortion regimens recommend a follow-up
ultrasound after the abortion has occurred. This examination can help determine
if any of the pregnancy materials remain.
- Complications of abortion with septic shock
- Complications
- If not treated promptly, septic shock can be fatal. It can cause organ failure and damage virtually any part of your body.
Typical complications include:
- Respiratory failure
- Cardiac failure
- Liver failure
- Kidney failure
- Gangrene (body tissues die due to loss of blood)
In cases where septic shock is caused by a septic abortion,
a total hysterectomy may be necessary to remove the source of the infection. A
total hysterectomy removes the uterus, cervix, fallopian tubes, and both
ovaries.
Diagnosis of abortion with septic shock
Diagnosis
A diagnosis of septic shock can be confirmed with
laboratory tests:
A blood test can identify bacteria in the bloodstream.
Your white blood count, blood oxygen level, and organ functions will also be
checked.
Samples from your urine, cerebrospinal fluid, and lung
mucus will be cultured and tested for bacteria. Tissue samples from wounds may
be tested.
CT scans may be performed to identify residual pregnancy
matter, obstructions, perforations, or foreign bodies.
A chest X-ray may be done to check for fluid in your
lungs or pneumonia.
An electrocardiogram (ECG or EKG) may be done to identify
abnormal heart rhythms. An EKG monitors your heart rate. Electrodes are taped
to your chest to send the sound of your heart to the monitor. This can help
determine whether the heart’s blood supply is affected.
Treatment and recovery
Treatment
Septic shock is a medical emergency that must be treated
immediately. Because of the urgency, treatment often begins before the test
results can confirm the diagnosis. If you have signs of septic shock after an
abortion, you must be admitted immediately to an intensive care unit.
Successful treatment for septic shock is centered on two
goals: protection of the vital organs and removal of the source of the
infection.
Antibiotics are given first. Test results identifying the
specific bacteria that are causing sepsis can take a few days. To improve the
chances of killing the bacteria, two or three antibiotics may be combined.
Typical antibiotic treatment involves a combination of:
Typical antibiotic treatment involves a combination of:
- Ampicillin
- Gentamicin
- Clindamycin or metronidazole
The treatment can be refined once the specific bacteria
are identified. Your chances of surviving septic shock increase when you
receive antibiotics soon after the abortion.
Your treatment may include:
- Mechanical ventilation (breathing machine)
- Medication (to increase blood pressure)
- Intravenous (IV) fluids (to increase fluid in the bloodstream and blood pressure)
- Oxygen
- Hemodynamic monitoring (evaluation of heart and lung pressure levels)
In some cases, surgery is necessary. A complete hysterectomy may be performed if the infection is caused by matter from an abortion.
In some cases, a laparotomy may be performed. A
laparotomy is an incision in the abdominal wall that allows for quick access to
the abdominal cavity. This may be needed if your physician suspects the
infection is caused by:
- Uterine perforation
- Bowel injury
- Abscess
- Soft tissue infection
- Prognosis
- Outlook
- Septic shock, regardless of the source, has a high mortality (death) rate. Specific Circumstances can affect successful treatment. These include:
- Age
- Overall health
- Degree of organ failure
- Timing of the start of medical treatment
How to prevent septic shock
Prevention
Many cases of septic shock can’t be anticipated or prevented. You can reduce your risk by following these precautions:
Many cases of septic shock can’t be anticipated or prevented. You can reduce your risk by following these precautions:
- Consult with a licensed physician or clinic to pursue an elective abortion.
- Follow the directions exactly as provided for a medical abortion.
- Never attempt a self-induced abortion.
- Be aware of the signs of bacterial infection after any type of abortion.
- Pursue treatment for an infection as soon as possible.